How We Got Concussions So Wrong
Reading Time: 13 minutesAs Concussion Science Transformed, an Insidious Myth Took Hold. Many Doctors Still Believe It., I got a concussion. I didn’t get better. It turned out even my doctors had bought into a powerful myth., Concussion: there’s an insidious myth about a common sp
The first time Conor Gormally got a concussion, he felt as if he were standing on a ship at sea. A high school soccer player, he had decided to try out something new during his off-season: wrestling. His very first opponent caught him off guard, with a headbutt to the temple. ‘I stood up, then my horizon tilted to a 40-degree angle and I fell to the ground,’ Gormally told me years later.
He felt the room tip and roll. Emotions welled up from out of nowhere. ‘I was sobbing and saying, ‘I don’t know why I’m crying. I’m not upset. I’m just confused. I don’t know what’s happening here,’ ‘ Gormally recalled.
After examining Gormally, the school athletic trainer told him to go home and rest. Gormally’s primary care provider said the same thing, adding that he shouldn’t return to school or practice until his symptoms resolved.
Gormally dutifully followed their advice. He turned off the lights in his room, drew the curtains, climbed into bed, and rested. And rested. And rested.
Weeks passed. The fall semester ended. Gormally still wasn’t better. He was exhausted and had a headache around the clock. His emotions continued to be all over the place. One moment, he would feel totally numb; the next, he would get overwhelmed and start crying. He tried going to a movie with his mom and girlfriend. The sounds and lights were an assault—he went home nauseated, with a pounding head. Wasn’t the rest supposed to be helping?
When Gormally visited his primary care provider a second time, the doctor told him to just keep resting. The doctor wrote in the appointment notes, which Gormally later requested, that Gormally was ‘frustrated’ and his mother was ‘overbearing’ and ‘overly worried.’
After almost two months, Gormally was finally well enough to go back to school—and ready to put the whole experience behind him. But he kept getting concussions. Three more times over the next three years, he hit his head playing sports: twice in soccer, and once during Ultimate Frisbee. With each concussion, he received the same spiel from medical providers: ‘There’s not much we can do for you.’ ‘Go home and rest.’ ‘These things tend to get better on their own.’ Each time, it didn’t feel as if they did.
There was a reason the ‘just rest’ advice worked so poorly for him. For years, doctors had been told that concussion patients needed total rest in order to recover. But around the time of Gormally’s concussions, which occurred between 2013 and 2016, the science was beginning to indicate the opposite—patients who ‘cocooned’ themselves in a dark room, even for only a few days, consistently took longer to get better than people who stayed engaged with their daily activities.
Since then, study after study has shown that the concussed brain requires active rehabilitation—activities like exercise, reading, and screens—to heal. The most up-to-date Consensus Statement on Concussion in Sport, a report prepared by an international panel of experts, recommends ‘active rehabilitation’ and discourages total rest. As with most injuries, the specifics of what that rehabilitation looks like varies from case to case; researchers and specialists have an arsenal of protocols and therapies at their disposal.
You’d think that this would have meant a revolution in how doctors understand and treat concussions. It hasn’t. For many patients, not much has changed at all. A report published in 2018 found that more than half of patients with concussions—millions a year in the United States, according to the Centers for Disease Control and Prevention—are still leaving the doctor’s office without actionable, evidence-based information or referrals to specialists. Instead of that crucial step, many patients, to their detriment, are still being told to simply cocoon.
That’s the advice I got last May. During a pickup game of soccer, a ball slammed into my head, shattering my sunglasses and giving me the immediate feeling that everything around me was happening in 2D. Over the following days, then weeks, everything felt gauzy and sore. My normally chatty internal monologue was quiet. I had a constant feeling of pressure behind my eyes. Cooking, reading, and cleaning may as well have been linear algebra.
No fewer than three medical professionals told me that a concussion was a ‘bruise to the brain’ and that I needed to rest as much as possible for it to heal. Their definitions of rest were all slightly different, from blinds-drawn sensory deprivation to short walks. But all told me that if my symptoms got any worse, I needed to immediately stop whatever I was doing—otherwise, I risked drawing out my recovery.
‘It’s a huge myth,’ Gormally told me. In 2018, after his experience, he and his mom founded Concussion Alliance, a nonprofit that is dedicated to patient and provider education. ‘It’s so pervasive; it’s actively damaging people’s recovery.’ The idea that cocooning may be harmful is completely new information to most patients Gormally meets. Concussion experts I spoke to say it’s probably not a coincidence that half of concussion patients continue to experience symptoms months after the initial hit.
That was me. It was four months after my concussion—months in which I lost income and watched, from bed, as my summer slid away—before I could say I was mostly recovered. The way I ended up with the information I needed to heal felt like sheer luck. In the aftermath, I was still reeling. I wanted to understand: How did we get concussions so wrong in the first place? And how many patients were still being told the wrong thing?
As long as humans have been hunting and gathering, playing and fighting, we’ve been bonking our heads. But until the 1990s, we treated these bonks—the ones that do not outwardly appear to damage anything—as if they were no big deal. ‘No one recognized that concussions were dangerous. We just sent people back onto the field, or into a war zone,’ said Mary Alexis Iaccarino, a physiatrist specializing in concussion recovery at the Massachusetts General Hospital Youth Sport Concussion Clinic. Athletes were allowed to accumulate hit after hit; workers were expected to be on their feet all day while their heads were still swimming. ‘That was bad,’ said Iaccarino. ‘That is still bad.’
It’s largely because of football that we’ve started clocking how life-altering concussions can be. Throughout the 20th century, there had been isolated reports of athletes developing a constellation of disabling symptoms: depression, mood swings, rage, drug addiction, and memory problems. The first mention of the disease, published in JAMA in 1928, labeled it ‘punch drunk syndrome.’ By the 1990s, amid growing concern about concussions and their extended impacts, the NCAA and NFL began funding long-term research into the epidemic.
The 2002 death of NFL Hall of Famer Mike Webster, who had suffered a lengthy cognitive decline, brought concussions into the spotlight. When neuropathologist Bennet Omalu conducted Webster’s autopsy, he discovered tangles of proteins dislodged from Webster’s brain cells by thousands of hits. Autopsies of dozens of other players revealed the same phenomenon. He called the condition chronic traumatic encephalopathy.
It’s worth mentioning that CTE is vanishingly rare, even among athletes. But the disease’s discovery and the epidemic of postconcussion symptoms among football players helped usher in a drastic change in the way we treat concussions generally. Instead of hustling people back out onto the field, doctors began pushing rest. Between 1999 and 2001, high school and college football players were returning to the field just three days, on average, after getting a concussion, according to an analysis published in the British Journal of Sports Medicine. By 2014, they were waiting 13 days. Studies showed that rats with brain injuries performed worse in cognitive tasks and produced less of a protein important for brain healing when they were forced to run on a wheel vs. when they were allowed to do whatever they wanted, whether that was exercising or just chilling out. Other studies showed that humans tended to feel better if they didn’t immediately returning to work after a concussion.
It’s one thing to avoid immediately going back onto a football field, where you might get hit again before you’ve recovered, or to work, which might be cognitively straining. But instead of nuanced advice that included downtime or a scaling back of activities, the recommendation became total rest. In 2009 the third Consensus on Concussion in Sport listed ‘complete physical and cognitive rest until symptoms resolve’ as the first line of treatment for a concussion. Doctors began telling patients to draw their blinds, close their eyes, and return to their lives only when they felt better. ‘We swung the pendulum completely in the other direction,’ Iaccarino said.
Immediately after a person gets a concussion, resting in a quiet, dim place can feel good—and for some individuals, a day or two of this might be helpful for recovery. Then there’s the tendency to conflate concussions, which are considered mild traumatic brain injuries, with more severe conditions, like penetrating head injuries or brain hemorrhages. In those cases, many patients benefit from a very quiet environment. ‘We were trying to apply concepts globally, and it may not have been the right thing,’ Iaccarino said.
The days immediately after my concussion weren’t too bad. It was a long weekend, so I hadn’t had a chance to speak with a doctor. I went home and slept for a few hours, then walked to the grocery store. I slept some more. I went on a first date, where I ordered a virgin piña colada. Then I took a nap. Sure, I was exhausted, and the summer sunlight was painful when I didn’t wear shades, but I figured I was taking a path of moderation.
On Monday, I was getting ready to start work when I thought to call a physician. On that phone call, I was told that I had been going about my recovery all wrong—I needed to be in bed. So I put my phone away, turned on some calming instrumental music, and lay down. That’s how I stayed for the next month.
We think of concussions—partly because doctors say it so often—as a ‘bruise to the brain.’ But that’s not quite right. It doesn’t capture the cascade of changes that happen inside the skull during and in the aftermath of a blow to the head.
Imagine this instead. Your brain is Jell-O sitting inside a mold: your skull, with a viscous layer of cerebrospinal fluid holding it in place. If that Jell-O shakes, it doesn’t slosh. On the inside, it’s twisting back and forth. ‘It deforms,’ said Christina Master, a pediatric sports medicine and brain injury doctor at Children’s Hospital of Philadelphia who specializes in concussions. As your brain jiggles and twists, neurons—the long, cordlike cells that transmit signals in the brain—stretch and fray.
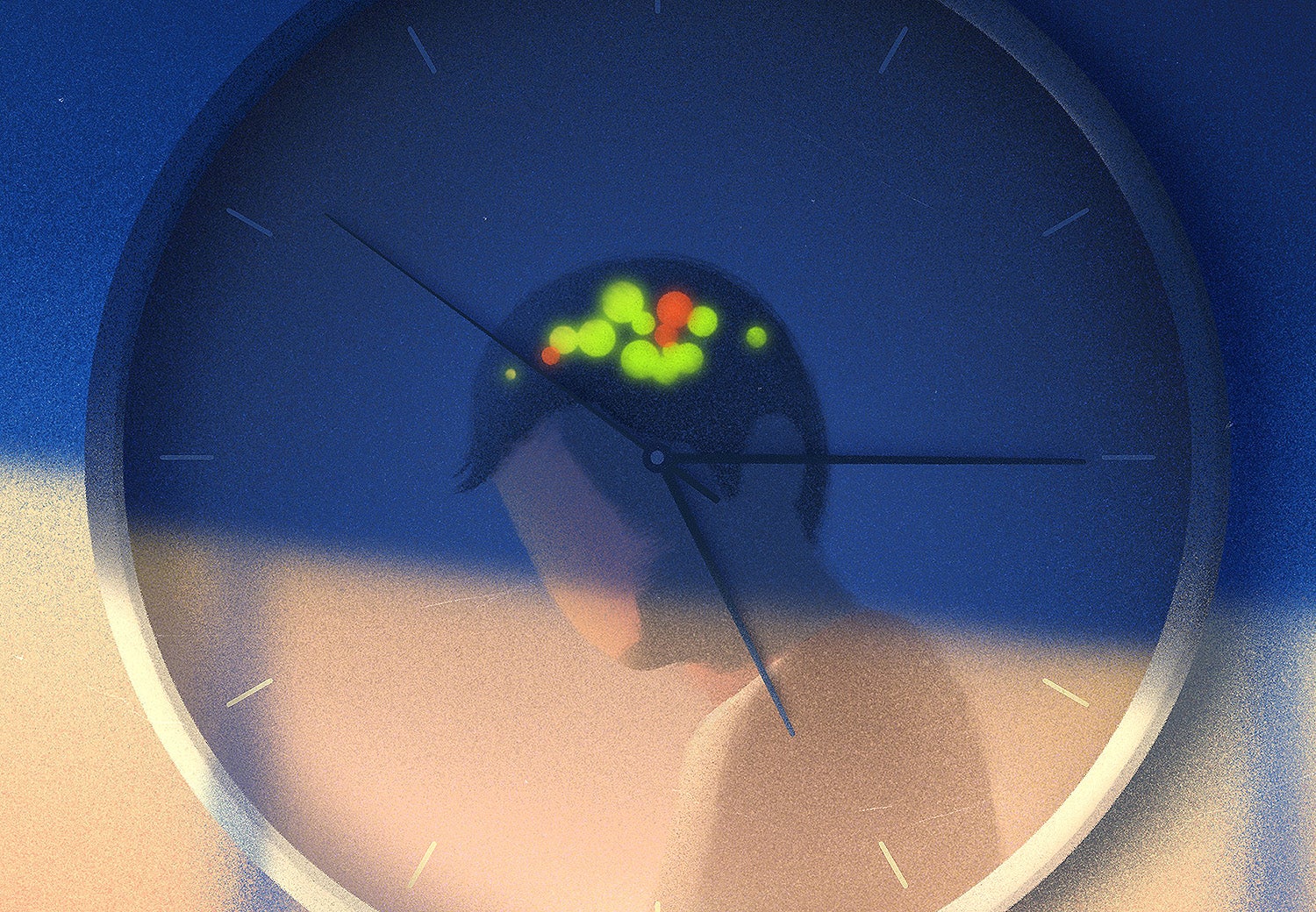
Without those pathways, communication within the brain becomes chaotic. You might open your email and see a scramble of words, struggle to organize the steps in a recipe, or try to jog only to forget where your limbs are in space. ‘The regions of the brain aren’t talking to each other properly,’ said Fatima Nasrallah, a neuroscientist at Queensland Brain Institute in Australia.
These neurons are terrible at repairing themselves, said Henrik Zetterberg, a professor of neurochemistry at the University of Gothenburg in Sweden. But it turns out that to heal from a concussion, your brain doesn’t actually need to stitch together those damaged connections. When a major highway needs roadwork, commuters don’t just wait around until it’s complete. Instead, traffic gets diverted. That’s what happens after a concussion, Zetterberg said. When brain cells stretch and fray, signals get sent down other neural pathways. At first, this is incredibly taxing. You might feel exhausted, have pounding headaches, and be emotionally frazzled. You might struggle to complete tasks that once felt easy, like reading or doing basic math. Then, eventually, you might start to feel better. ‘That is not because the brain has healed,’ Zetterberg said. ‘It is because the brain circuits that are not injured, they recalibrate themselves.’ The brain finds new highways to send signals down.
During that recalibration period, you may have to go easier on yourself. But that recalibration can’t happen while you’re lying in bed in a dim, quiet room.
Total rest—the kind where you’re lying in bed all day, doing nothing—generally isn’t good for the body or the mind. People on bed rest lose muscle mass, have a slowed-down metabolism, and become dehydrated. This protocol can even delay recovery in patients critically ill from heart disease or suffering from rheumatoid arthritis. Concussion patients aren’t told to just rest in bed—they’re often encouraged to go through a period of sensory deprivation. ‘In a lot of places, that’s torture,’ Iaccarino said. ‘It induces things like depression, light sensitivity, noise sensitivity, physical deconditioning.’
The recognition that total rest is detrimental to so many other conditions made researchers start to question whether it was truly helping concussion patients. But the medical world has been slow to catch up.
Four weeks into my concussion recovery, my routine hadn’t changed much. Each day, I woke up, drank my coffee, ambled the half-mile around the pond near my house, then lay down and listened to two episodes of the podcast Normal Gossip, which I rationed out so that I had something to look forward to. Then I napped. And napped. And napped. I wasn’t getting better. In fact, I was getting worse.
The first studies that asked participants to exercise through their concussion symptoms were controversial. ‘People were worried you’d do serious permanent harm,’ Iaccarino said.
In 2009 Canadian researchers recruited 16 children and teenagers between the ages of 10 and 17. All had endured concussions; all had initially followed their doctors’ advice to rest; and all were still suffering from symptoms four or more weeks later. Every day, the researchers had the children do 15 minutes on the treadmill or stationary bike at about 50 percent of their maximum effort, then 10 minutes of drills for their respective sport. If the kids’ symptoms ramped up during a session, they were told to stop. Within five weeks, on average, the children and teens made complete recoveries.
Then, in 2016, a JAMA study of more than 2,400 young athletes found that among those who followed a strict resting protocol, 43.5 percent still had symptoms after 28 days. Among those who resumed activity within the first week, sometimes in spite of symptoms, that proportion fell to 24.6 percent.
Gradually, other studies added to the evidence that people who engage in activity—even in the hours immediately after their concussion—fare better than those who didn’t. The activity in question doesn’t even have to be physical. A 2022 study published in the journal Pediatrics found that children who spent less than two hours a day on screens in the first week after a concussion had worse concussion symptoms after one month than did those who engaged in ‘moderate’ screen time of two to seven hours a day.
It’s important to note that no one was asking concussion patients to throw themselves back into a football game or immediately return to work full time. We’re talking a moderate amount of activity, in a setting where they were not likely to get hit on the head again and which they were encouraged to scale back if they felt they needed to. But that was far more than the recommendation at the time—or the recommendation that many patients, like me, are still given today.
‘Your brain needs to get back in shape after a concussion,’ Master said. Sometimes, that means dealing with a small amount of discomfort. As an analogy, Master likes to point to the soreness you might experience after a productive workout: ‘If you’re not getting a little sore with your workout, you’re not actually making good progress.’
Here is what getting in shape can look like after a concussion: For the first 48 hours, concussion experts recommend, you should get ‘relative rest.’ Sleep a lot—as much as you need. Maybe cook a meal. Watch a TV show. Chat with your friends. It’s OK to do all this despite symptoms, but if they worsen by more than just a bit, that’s a sign to back off. This is basically what I did when I was left to my own devices—before I consulted a doctor.
After that 48-hour period, it’s time to start gradually acclimating yourself back to your normal activities, albeit at a lower intensity and shorter duration (and with guidance from a specialist). At first, that might involve a brisk walk or going through your inbox; later, perhaps, a short jog or a few hours of work. The key thing is, the activity shouldn’t worsen your symptoms by more than 2 points on a scale of 1 to 10, according to the sixth Consensus on Concussion in Sport.
I wasn’t acclimating myself back to activities. I was lying in bed. It didn’t even occur to me that this was the wrong thing to do until another science writer I told of my condition replied: ‘I had a concussion last year. One thing I learned is that rest works for some people, but sometimes it’s not enough.’ She passed along an episode of the podcast Ologies that featured an interview with a specialist in traumatic brain injuries, and recommended seeing a vestibular physical therapist—someone who specializes in the body’s sense of balance. It took me weeks to take the recommendation, and when I did, I had to pay almost $200 out of pocket per session.
It was worth it. On Day 1 of my treatment with her, the therapist put me on a treadmill and strapped on a heart rate monitor as we watched my symptoms. ‘Let me know when you’re at a 5 out of 10,’ she told me. ‘Tell me your heart rate. Now hold that for 20 minutes.’ We did strange exercises for my brain, eyes, and ears—all the systems that the flying soccer ball had knocked out of whack. I stood on one foot while tracking a swinging ball with my eyes, I did word association while walking backward, and I completed memory exercises.
Once a week, I went back. And each morning in between appointments, I diligently followed the routine she gave me, jogging at the target heart rate for 20 minutes, standing with my roommate in the kitchen doing word association and eye tracking. Finally, the physical therapist and I made a list of goals. At the top was getting back to work. At first, she had me working for 30 minutes. If my symptoms didn’t increase more than 2 points, I could add another 30 minutes a day. As I healed, she cleared me to go for bike rides, go camping, see the band boygenius in concert, and even kick the soccer ball around with friends. Three weeks later, I was 90 percent better.
Compared with many patients, I got lucky. In a cohort study of 831 people who showed up in the emergency department after a concussion, published in JAMA Network Open, only 44 percent of participants received follow-up care within three months of their injury. Of those who did receive follow-up care, only 15 percent ever visited a clinic specializing in brain injuries, like the one that treated me.
Months of reporting taught me that if I had received follow-up care within the first week or two of my concussion, my year could have looked very different. Perhaps I wouldn’t have turned down months of work, draining my savings account in the process. Perhaps I would have been able to take that road trip to Montana and backpack Mount St. Helens. I was angry. I am still angry.
I saw that indignation reflected in Conor Gormally and his mom, Malayka, who runs Concussion Alliance with him. Together, they have spoken to hundreds of patients. ‘Where was that actionable information?’ Conor said. ‘There just wasn’t any.’ Conor was going through his concussions at a time when there was less firm research into recovery than there is now, before the medical consensus emphasized active rehabilitation. Even still, there were signs in the literature that resting might not be enough and that he was right to be, as his doctor had written, ‘frustrated.’
The thing is, I wasn’t sure where to direct my anger. Neither the Gormallys nor I blamed our primary care doctors. According to a review article published in the International Journal of Environmental Research and Public Health, between 8 and 38.4 percent of medical school students in the United States and Canada report never being taught about concussions, and between 16.8 and 24 percent have no memory of learning about concussions. Recently, Conor gave a guest lecture to a crowded hall of second-year medical students. Afterward, the program director pulled Conor aside and said, ‘That’s probably more than they would have gotten through their neurology courses.’
Should I be angry at those medical schools? Or does the blame lie with our insurance system, which didn’t cover my $200-a-pop physical therapy appointments? What about the culture of primary care and emergency medicine, in which chronic-but-not-life-threatening conditions are shunted to the side in favor of those that can be stabilized with a procedure or pill?
I still don’t have an answer, and neither do the Gormallys. Sometimes, change is just frustratingly slow. A often quoted statistic holds that medical research takes 17 years, on average, before it transforms care for patients—just about the amount of time that has elapsed since research began to support the importance of active rehabilitation for concussions.
The way medicine treats concussions is beginning to change—slowly, but on schedule.
The Concussion Alliance designed a continuing education course on patient-centered concussion care for primary care providers and emergency physicians. The class, run by an accrediting organization, teaches the providers about the importance of follow-up care. Policies requiring concussed child athletes to receive medical clearance before returning to play rolled out; this sent a wave of concussion patients to children’s hospitals, motivating pediatricians to figure out how to help them beyond just ‘Rest until you feel better.’ Researchers are developing tools to help identify concussions—allowing doctors to get a firm diagnosis—and track the brain’s healing process. Advocates like the Gormallys are making sure patients get that actionable information they couldn’t find before.
As long as people play sports and go to work, drive cars and stumble down stairs, we’ll keep injuring our brains, as we do other parts of our bodies as we move through the world. But maybe, in the near future, when another average pickup soccer player hits his head, the doctor will tell him that his brain isn’t bruised—it just needs a little rewiring. And the soccer player will walk out knowing exactly what to do.
Reference: https://slate.com/technology/2024/03/concussion-symptoms-signs-treatment-advice.html
Ref: slate
MediaDownloader.net -> Free Online Video Downloader, Download Any Video From YouTube, VK, Vimeo, Twitter, Twitch, Tumblr, Tiktok, Telegram, TED, Streamable, Soundcloud, Snapchat, Share, Rumble, Reddit, PuhuTV, Pinterest, Periscope, Ok.ru, MxTakatak, Mixcloud, Mashable, LinkedIn, Likee, Kwai, Izlesene, Instagram, Imgur, IMDB, Ifunny, Gaana, Flickr, Febspot, Facebook, ESPN, Douyin, Dailymotion, Buzzfeed, BluTV, Blogger, Bitchute, Bilibili, Bandcamp, Akıllı, 9GAG